Some people with type 1 diabetes (T1D) find current treatment options to be inadequate and unsatisfactory and have taken it upon themselves to design technological solutions which work for them.
Tired of waiting for commercial solutions that meet their needs, patients are constructing their own Do-it-Yourself Artificial Pancreas Systems (DIY APS). Although still confined to a relatively small group of users, the use of these systems is becoming more widespread; and their development and uptake has left the clinical community playing catch-up.
DIY APS users (sometimes known as ‘loopers’) are being seen in clinic by their healthcare team and still need advice and help to manage their diabetes. Yet there is almost no clinical, ethical, or legal guidance to help healthcare professionals, in particular clinicians, to appropriately support patients who choose to (or might want to) loop.
Why is innovation in diabetes treatment needed?
Innovation with regards to T1D treatment has been a slow process. Standard treatment consists of self-injecting insulin multiple times a day. Users have to prick their fingers to draw blood, measure the levels of glucose in it with a blood glucose meter, and determine the dose of insulin to inject.
The problem with this treatment regime is that it can be onerous, with continual self-management taking its toll on patients. First of all, self-injecting insulin multiple times a day is time-consuming and inconvenient. Secondly, determining the correct dose of insulin isn’t always a straightforward task. Patients must decide how much insulin to inject based on their blood glucose levels and a host of other factors, such as the type of meal eaten or the amount and type of exercise they expect to do.
In recent years two medical devices have begun to alleviate the burden of diabetes self-management. These are continuous glucose monitors (CGM) and insulin pumps. A CGM is a sensor which sits under the skin and measures the glucose levels in the fluid that sits between the cells of our body. The CGM then transmits the data to a reader (e.g. a smartphone). The sensor can sit under the skin for up to 10 days and take readings hundreds of times a day. Insulin pumps, as their name suggests, are devices which pump insulin. Insulin pumps are small devices which can be programmed to deliver insulin at a set rate throughout the day and to deliver extra doses at mealtimes. Insulin pumps allow users to receive low levels of insulin continuously, helping them maintain their blood glucose levels in a healthy range.
Together these two technologies can help alleviate some of the burdens of T1D (e.g. the need to finger-prick and the need to inject multiple times a day). However, what they don’t do is ease the on-going and continuous necessity of making complex decisions about the amount of insulin to administer in different circumstances.
As well as being cognitively demanding, having to determine how much insulin to inject can also be anxiety inducing. The reason is that the stakes are high. Administering too much insulin can lead to low blood glucose (known as hypoglycaemia) which, if untreated, can lead to a diabetic coma and, eventually, death. Administering too little insulin results in high blood glucose levels (known as hyperglycaemia) which can lead to diabetic ketoacidosis. If untreated, this can be fatal. In the long term, elevated blood glucose levels can lead to further complications, including kidney damage, nerve damage, and vision loss.
What are DIY Artificial Pancreas Systems?
DIY APS are systems made up of four interconnected components:
- a smartphone or small computer on which to run an algorithm, collect and display data, and issue commands;
- a CGM to provide ‘real time’ glucose data;
- software (AndroidAPS, OpenAPS, or Loop) to interpret CGM readings, perform calculations and send instructions to insulin pumps; and
- an insulin pump to administer insulin therapy based on commands received from the smartphone.
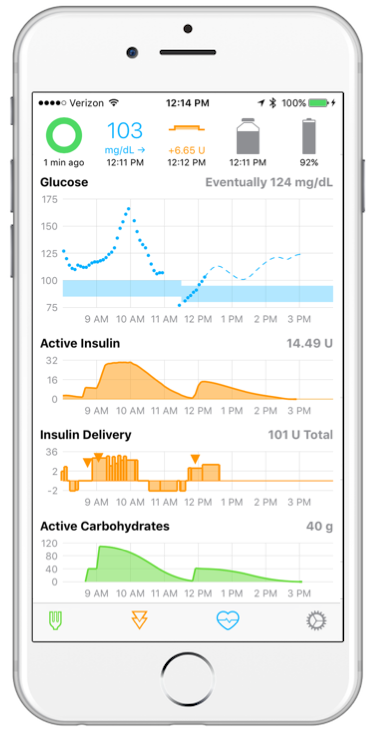
Connecting these components together creates a hybrid closed loop system, which automatically adjusts and administers insulin doses, something which users report offers greater overall blood glucose control and decreased anxiety relating to potential hypoglycaemic episodes (including during sleep). Significantly, DIY APS allows users – known as ‘loopers’ – to delegate some of their decision-making to the algorithm, decreasing the amount of cognitive effort and time spent self-managing their disease. So how does it do this?
The DIY APS algorithm determines the dose of insulin to administer and issues a wireless command to the insulin pump to administer it. This process continuously repeats itself, with the algorithm adjusting the delivery of insulin as it receives new data from the CGM. DIY APS is a hybrid rather than fully closed loop system, because users still need to ‘announce’ meals to the system. This manual inputting of data is then fed into the algorithm along with the data gathered from the CGM.
DIY APS are not regulated medical devices and they cannot be purchased commercially. Instead users have to build the system themselves using the required hardware and instructions available on the internet. This includes acquiring compatible CGMs and pumps if they don’t already have these. Depending on which APS they are building (there are 3 currently available as mentioned earlier), they may also need a small computer (Raspberry Pi or Edison board), and a small piece of kit called a RileyLink to ensure the different part of the system can communicate with each other.
Setting up the system requires a measure of technical know-how, but there is an online community of fellow users who work to debug the system, post updates, and help with any problems people have setting up their DIY APS. The community also hosts build events, where users meet offline to help each other build the systems, troubleshoot problems and share expertise.
The challenge facing doctors
The problem facing doctors is that no regulatory body has approved the use of these DIY systems and they have not been through the stringent safety checks required of medical devices. Doctors may not even have heard of this technology. But their patients are already using it and reporting good results. Since doctors are legally and professionally responsible for providing safe care to their patients, this can put them in a difficult position.
In their quest to provide effective and clinically appropriate treatment, should doctors assist their patients in their use of these unregulated DIY systems? After all, despite only having a small community and evidence base, DIY APS users are remarkably satisfied with the outcomes of their DIY endeavours.
Should doctors actively encourage patients to build DIY APS, or discourage it due to safety concerns surrounding these unproven systems? Ought they continue to prescribe the relevant components (CGMs, insulin pumps, and so on), knowing that patients are using them in this manner? Would it be more problematic to change the prescriptions in an attempt to prevent this usage? What about where parents have built these systems for young children who are unaware of the risks?
As the number of DIY APS users steadily increases, doctors are increasingly concerned about what appropriate care for these patients looks like.
A new horizon?
DIY APS is signalling a shift away from the traditional ‘doctor-knows-best’ landscape. It’s even going a step further than current shared decision-making models. We are now seeing empowered patients taking control and expecting their doctors to follow their lead. What is clear is that this technology raises a number of important and pressing questions; for example:, .
- Are individual clinicians liable because they prescribe relevant technology (CGM and Insulin Pump) which the patient is using off licence?
- If patients are using their prescriptions inappropriately, do clinicians have a duty to withdraw these devices/not give prescriptions for consumables?
- Are clinicians who assist users of DIY systems in breach of their professional and/or ethical duties?
- As the saying goes, with great power comes great responsibility. Is now the time for patients to be ultimately responsible for any harm (and benefits) they experience as a result of DIY treatments?
It is these questions, amongst others, which we start to explore in a series of forthcoming blog posts.
Written by Joseph Roberts, Victoria Moore, and Muireann Quigley.
Funding
Work on this was generously supported by Wellcome Trust Investigator Award in Humanities and Social Sciences 2019-2024 (Grant No: 212507/Z/18/Z), an ESRC Impact Acceleration Award, and a Quality-related Research grant from Research England.
