Nana Sartania and Emma Bailey, University of Glasgow

In 2015 Dr Enam Haque (University of Manchester) conceived the idea of establishing a Forum whereby academics and outreach practitioners, charitable organisations and postgraduate medical colleges from across the country would come together to identify current and emerging issues in widening participation (WP) and share knowledge and good practice in order to understand the issues students from a WP background face when accessing and succeeding at Higher Education institutions. This National Medical Schools’ Widening Participation Forum, NMSWPF, has since evolved into a vibrant, collaborative organization with a shared vision. NMSWPF performs research on admissions policy and outreach, and by sharing good practice and discussing new ideas, ensures that colleagues across 24 universities, the Medical Schools Council Selection Alliance, voluntary organisations and postgraduate medical colleges are all working towards establishing practical solutions to address the issues. Dr Clare Ray from the University of Birmingham has served as the Chair of this Forum since June 2021.
Widening participation is multifaceted – while the focus in the UK concentrate mostly on students from low socio- economic backgrounds, the list of WP indicators (‘flags’) the universities use is much wider. Applicants with care experience or from target schools with low progression rate to Higher Education or, students with certain disabilities are often considered separately by the admissions teams and contextual offers may be used to recognise additional challenges to their pre-18 education. But to ensure equitable treatment of all applicants at the participating Medical Schools it is necessary to formulate objectives and policy, and to measure whether those policies have the desired impacts. Discussion, collaboration and coordination are essential to achieve this and that is the central mission of NMSWPF.
The Forum is best placed to look into the issues the societal inequality poses for students from lower socioeconomic background as all the members of the organisation are educators who work with students in academic or support roles and guide them throughout their medical journey. They understand the barriers these students face and are eager to help find practical solutions to address the disadvantage.
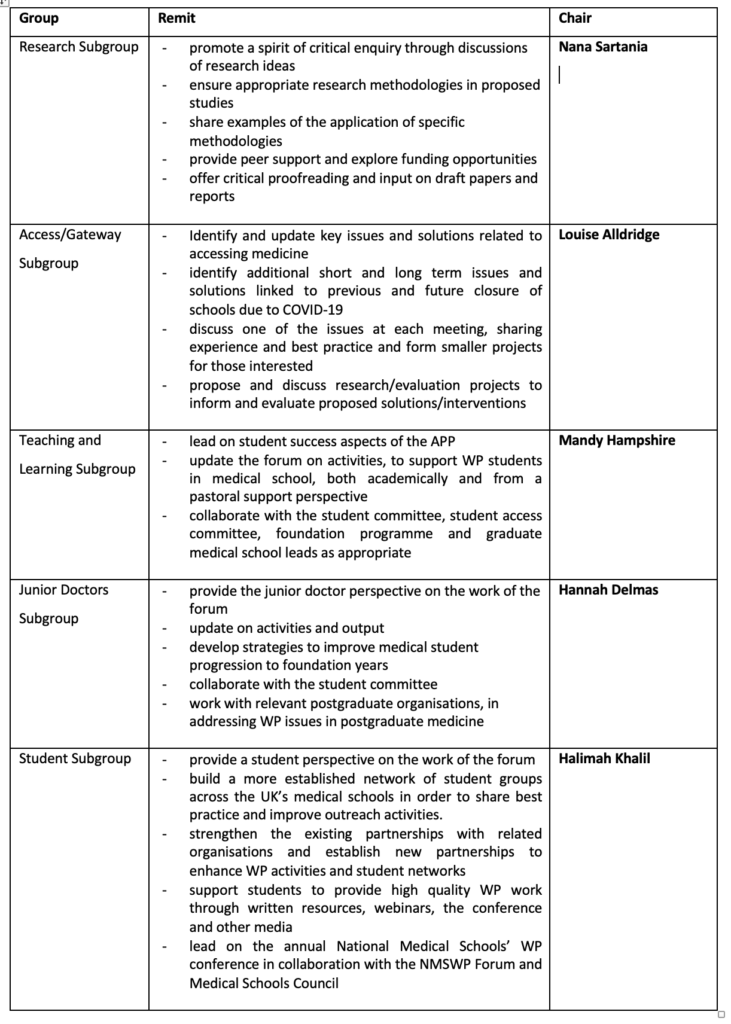
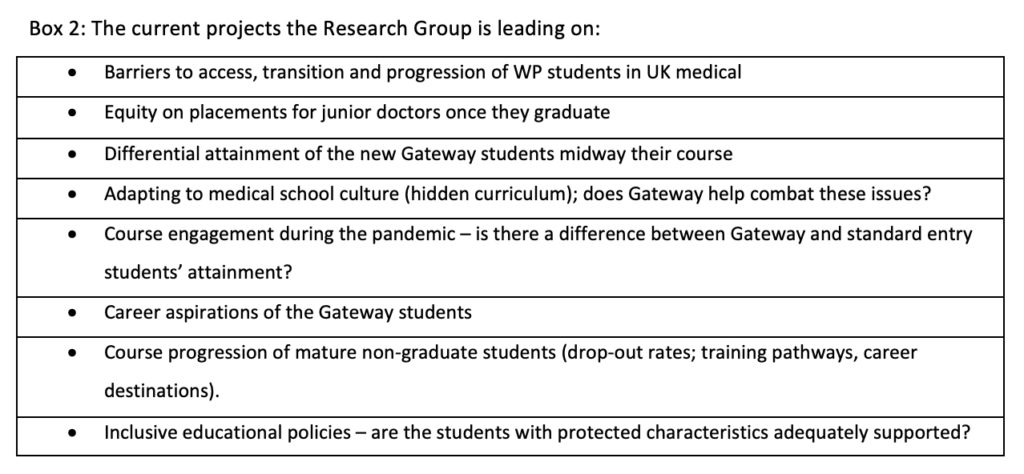
The Forum has a number of subcommittees, each with its own remit (see Box 1), all working towards developing an evidence base for successful interventions to tackle gaps in not only the access to Medical School but also their success after admittance to the course, and beyond. Central to the work of each subcommittee is the research group (chaired by Dr Sartania). The research group aims to promote a spirit of critical enquiry through discussions of research ideas and ensures that appropriate research methodologies in proposed studies are used so that valid conclusions can be reached. The Research Committee encourages colleagues to develop new studies in the field of widening participation and believes that with such a wide reach, the Forum is best placed to explore the issues – we have broad and varied expertise among the 100+ members, who are passionate about the issues we discuss in the meetings and helping to achieve a more diverse and inclusive Medical profession for the UK. We want to conduct relevant research, with sound methodologies, and support colleagues wishing to explore funding opportunities or apply for Ethical approval. We are keen for new members to come forward with research proposals and initiatives and want to help them refine their project ideas and bring proposals to fruition. This extents to critical input on draft reports and publications, which is usually much appreciated by academics striving to engage in this kind of educational research.
We also place a great deal of importance on the work of the Students’ and Junior Doctors’ subcommittees. The insight these groups provide into the everyday problems the WP students and the experience of graduates is authentic and first-hand. They will have discussed these issues with peers and will have thought about tangible solutions, so giving them a seat at the table is very important. What is also important is that these students and junior doctors have access to the specific groups we are targeting and are best placed to conduct focus groups with them to explore their views. One example of such interaction is a current study the junior doctors’ group is pursuing on how best to bridge the WP graduates’ transition from university into the workforce; it is especially important to see how different the views and expectations of a wide range of staff are from the views of the graduates themselves. If we compare and contrast the responses from colleagues who work with students from WP backgrounds (academics, clinical academics/NHS practitioners and professional services/outreach staff) and the ones from junior doctors, it becomes possible to remedy mismatches and facilitate a transition that is more successful and less stressful for all concerned.
The outcome of the forum-wide collaboration is already tangible – we have published a peer-reviewed article (http://eprints.gla.ac.uk/250141/1/250141.pdf), presented at an international conference (https://amee.assetbank- server.com/assetbank-amee/action/viewAsset?id=3630&index=0&total=26&view=viewSearchItem), initiated a survey of graduates (https://forms.office.com/e/by1GgRrY4v) and have secured access to a national database (UKMED) (https://www.ukmed.ac.uk/research). Our research projects span a wide range of topics from researching the barriers to access, transition and success of WP students in UK medical schools, to the subgroups’ work on differential attainment or on equity of placements for junior doctors once they graduate. The forum members are also interested to research how the WP students adapt to the medical school culture (‘hidden curriculum’) and whether the pre-entry courses (Gateway) help address issues medical students from a WP background experience (imposter syndrome; lack of knowledge of the training pathways; lack of confidence etc). We also want to look into the career aspirations of these students and whether/how these change throughout the undergraduate study.
The sharply rising inequality in the UK has brought the idea of social justice into sharper focus and led to the introduction of new initiatives by higher education institutions to tackle the problem. Medical schools are notorious in the degree of overrepresentation of students from higher socio-economic status, despite the fact that only 6% of the general population actually are from the top socio-economic classes (Savage et al., 2013; Thomson, 2016). There is overrepresentation from those who went to private schools and those whose parents are doctors. While only 7% of children in the UK attend private schools (Sellgren, 2014; Goodall, 2017), 27% of all medical school students are educated privately (Carrell, 2016; Coughlan, 2018; Rees et al., 2022). With respect to the Black, Asian, and Minority Ethnic representation, inequality is obvious from the stats here too – only 5% of doctors of all grades come from Black and Afro-Caribbean origin (NHS, 2021), while the number is even lower at the level of consultants (3%) – so, it is about fair distribution of the limited resources available (university education) and the need for it to be shared out fairly. The ultimate winners will be the patients in the end as a diverse medical workforce is much more able to understand the issues of diverse communities and therefore benefit their healthcare.
While the universities contribute their fair share to address the problem by utilising contextual admissions and WP programmes to prepare students for university, there is more to be done in terms of seeing these students through the system. Often the students struggle and require help from academic and support staff. So, understanding the barriers the students face, not only before but also after admission, is a necessity. We have conducted a forum-wide study to address the issue and found that the barriers are to a large extent linked to the social and cultural capital (supported by financial capital) that people from different backgrounds accrue. Applications for admission will inevitably reflect the background that the students come from and therefore it is vital that the staff are trained, and drawn from a wide pool of diverse backgrounds and provided with Equality, Diversity and Inclusion (EDI) training and a clear understanding of the school’s strategy on recruitment and support for WP students.
To conclude, the material circumstances the widening participation students grow up in influence the way they feel about themselves, and how they project themselves to others. Perhaps it is not easy to break those barriers but with the educational and employment opportunities they are pursuing, they will be able to address their disadvantage. Increased awareness of the issues these students face will hopefully mobilise medical schools’ staff (academic, clinical and professional services) to address social mobility issues and lead to practical, targeted support (e. g. financial support/bursaries, peer network/buddy system, mentoring, career guidance etc). But this may only happen if teachers and support staff are aware of the issues, and for that we, as a forum, have work to do. We need to create an evidence base that can inform the universities and help develop policies. Widening participation is an important societal problem that must be tackled to achieve social cohesion and a medical profession that can provide appropriate care for the full diversity of communities in the UK. At a time when economic inequality is increasing across the globe, a lack of social mobility puts a strain on social cohesion. Most people would engage in civic conversations to support government policies designed to narrow the gap between the classes. Given that the uneven distribution of power, opportunity, resources is the fundamental driver of this class difference, empowering policies (aka widening participation) are needed to create greater equality.
Nana Sartania is a Senior Lecturer at the University of Glasgow School of Medicine. She is a member of the INReSH (International Network for Researchers in Selection into Healthcare), ASME (Association for the Study of Medical Education), Medical Schools’ Widening Participation Forum and a member of the board of the Medical Schools Council’s Selection Alliance.
References:
Rees E.L., Mattick K., Harrison D., Rich A., Woolf K. (2022) ‘I’d have to fight for my life there’: a multicentre qualitative interview study of how socioeconomic background influences medical school choice, Medical Education Online, 27:1,2118121, DOI: 10.1080/10872981.2022.2118121
Sartania N, Alldridge L and Ray C. Barriers to access, transition and progression of Widening Participation students in UK Medical Schools: The students’ perspective MedEdPublish 2021, 10:132 (https://doi.org/10.15694/mep.2021.000132.1)
Sellgren K. (2014) ‘Salary premium’ for private school pupils. https://www.bbc.co.uk/news/education-28125416
Goodall, J. (2017). Narrowing the Achievement Gap: Parental Engagement with Children’s Learning Creating a Learning-CentredSchooling System. London: Routledge.
Carrell S. (The Guardian, 22 Jan 2016) Students from wealthy backgrounds dominate medical schools.
Coughlan S. (7 December 2018) Oxbridge ‘over-recruits from eight schools’ BBC News https://www.bbc.co.uk/news/education- 46470838
Follow the National Medical Schools Widening Participation Forum on Twitter @NMS_WP_Forum
